September 18
The AIDS Institute leads this observance day.
This day brings attention to the growing number of people living long and full lives with HIV and to their health and social needs.
HIV and Older Americans
In 2016, nearly half of people in the United States (US) and dependent areasa living with diagnosed HIV were aged 50 and older. Though new HIV diagnosesb are declining among people aged 50 and older, around 1 in 6 HIV diagnoses in 2017 were in this group.

New HIV Diagnoses Among People Aged 50 and Older in the US
and Dependent Areas by Sex and Transmission Category, 2017
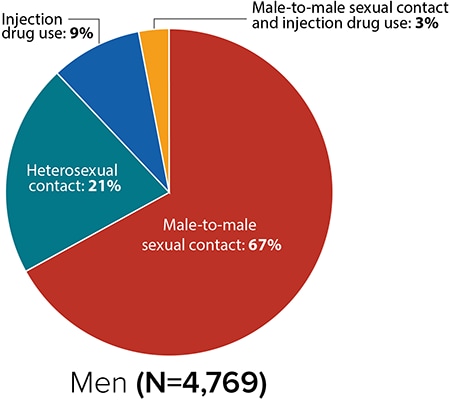

Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
New HIV Diagnoses in the US and Dependent Areas by Age, 2017
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
New HIV Diagnoses in the US and Dependent Areas by Age, 2017

Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
From 2012 to 2016, HIV diagnoses remained stable among people aged 50 and older in the US and dependent areas. But trends varied for different groups of older Americans.
HIV Diagnoses Among People Aged 50 and Older
in the US and Dependent Areas by Age, 2012-2016

Source: CDC. Estimated HIV incidence and prevalence in the United States 2010–2016. HIV Surveillance Supplemental Report. 2018;24(1).
Living With HIV
People Aged 55 and Older With HIV in the 50 States and District of Columbia

Sources: CDC. Estimated HIV incidence and prevalence in the United States 2010–2016. HIV Surveillance Supplemental Report. 2018;24(1).
CDC. Selected national HIV prevention and care outcomes (slides).
People With Diagnosed HIV in the US and Dependent Areas by Age, 2016

Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveillance Report 2018;29.
Deaths
In 2016, there were 10,944 deaths among people aged 50 and older with diagnosed HIV in the US and dependent areas. These deaths may be due to any cause.
Prevention Challenges
There are some behaviors that put everyone at risk for HIV. These behaviors include having anal or vaginal sex without protection (like using a condom or taking medicine to prevent or treat HIV), or sharing injection drug equipment with someone who has HIV. Factors that particularly affect older people include the following:
Older people in the United States are more likely than younger people to have late-stage HIV infection at the time of diagnosis, which means they start treatment late and possibly suffer more immune-system damage. Late diagnoses can occur because health care providers may not always test older people for HIV infection. Also, older people may not consider themselves to be at risk of HIV infection or may mistake HIV symptoms for those of normal aging and not consider HIV as a cause. Among people aged 55 and older who received an HIV diagnosis in 2015, 50% had been living with HIV for 4.5 years before they were diagnosed—the longest diagnosis delay for any age group.
Older people may have many of the same HIV risk factors as younger people, including a lack of knowledge about HIV prevention and sexual risk, such as having multiple sex partners. Older people also face some unique issues:
- Women who no longer worry about becoming pregnant may be less likely to use a condom and to practice safer sex. Age-related thinning and dryness of vaginal tissue may raise older women’s risk for HIV infection.
- Although they visit their doctors more frequently, older people are less likely than younger people to discuss their sexual or drug use behaviors with their doctors. And doctors are less likely to ask their older patients about these issues.
Stigma is a particular concern among older people because they may already face isolation due to illness or loss of family and friends. Stigma negatively affects people’s quality of life, self-image, and behaviors, and may prevent them from seeking HIV care and disclosing their HIV status.
Aging with HIV infection also presents special challenges for preventing other diseases because both age and HIV increase the risk for cardiovascular disease, lung disease (specifically chronic obstructive pulmonary disease), bone loss, and certain cancers. Older patients with HIV and their care providers need to maximize prevention efforts against these conditions and remain vigilant for early signs of illness. They also need to be careful about interactions between the medications used to treat HIV and those used to treat common age-related conditions such as hypertension, diabetes, elevated cholesterol, and obesity.
What CDC Is Doing
CDC and its partners are pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies among older Americans. Funding state, territorial, and local health departments is CDC’s largest investment in HIV prevention.
- Under the current funding opportunity, CDC will fund a national organization to support integrated HIV programs through the development of strategic national partnerships and enhanced communication efforts. This funding opportunity will also provide funding to health departments to engage community partners in a planning process to help develop jurisdictional Ending the HIV Epidemic plans.
- Under the new integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for HIV data collection and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the US.
- In 2019, CDC awarded a new cooperative agreement to strengthen the capacity and improve the performance of the nation’s HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions.
- Under the flagship community-based organization cooperative agreement, CDC awarded about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to people at greatest risk.
- CDC provides support and technical assistance to health departments and community-based organizations to deliver effective prevention and evidence-based interventions for antiretroviral therapy adherence for older Americans.
- Let’s Stop HIV Together (formerly known as Act Against AIDS), a campaign that focuses on raising awareness, fighting stigma, and reducing the risk of HIV infection among at-risk populations. Let’s Stop HIV Together includes resources and partnerships, aimed at stopping HIV stigma and promoting HIV testing, prevention, and treatment. Let’s Stop HIV Together empowers communities, partners on the ground, and health care providers to reduce stigma among all Americans, prevent HIV among the hardest-hit populations, and help people with HIV stay healthy. Campaign resources for the general public include the following:
- Stop HIV Stigma, which highlights the role that each person plays in stopping HIV stigma and gives voice to people living with HIV, as well as their friends and family. Campaign participants share their stories and call on everyone to work together to stop HIV.
- Doing It, which is designed to motivate all adults to get tested for HIV and know their status. Doing It delivers the message that HIV testing should be part of everyone’s regular health routine.
- Start Talking. Stop HIV., which focuses on gay and bisexual men and encourages open communication between sex partners and friends about HIV prevention strategies. It provides practical tools and tips to help gay and bisexual men share their HIV status, talk about condom use, medicines that prevent and treat HIV, and other prevention topics.
- HIV Treatment Works, which shows how people with HIV have been successful getting care and staying on treatment. It focuses on helping people with HIV stay healthy and live longer, healthier lives.
- Partnering and Communicating Together (PACT) is raising awareness about testing, prevention, and retention in care among populations disproportionately affected by HIV, including older Americans.
a Unless otherwise noted, the term United States (US) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
b HIV diagnoses refers to the number of people who received an HIV diagnosis during a given period of time, not when the people got HIV infection.